Caries
prevalence and experience of 12-year-old children in Montserrat
Coretta E.
Fergus
Introduction
The primary aim of this study
was to conduct an epidemiological survey of all 12 year olds on
Montserrat in order to:
- Determine the caries
experience
measured by the DMFT index and Oral Health Related Quality of Life
(OHRQoL) of 12 year olds
- To explore the differences
in
caries experience by gender, and socioeconomic status
No previous data could be found
on the oral health status of Montserratian people and the oral data
bank compiled by World Health Organisation (WHO) is devoid of any oral
health data for the island. With inadequate previous data this
investigation may be timely as it will provide some baseline data for
measurement of effectiveness of interventions to reduce caries in 12
year olds and could influence policy makers in the development of new
oral health policies.
Methods
Preliminary planning
Permission for conducting the
survey was sought and granted by the Ministry of Education (MOE) in
Montserrat and also from the principal of the Montserrat Secondary
School. Consent letters were distributed to the relevant children on
behalf of the researcher.
Training and calibration
Separate training and
calibration were carried out in line with BASCD guidelines for the
conduct of surveys of child dental health [1] and [2]. [These numbers
refer to the numbered list of references.] The calibration
was conducted at the Lister Primary Care Centre in Peckham where
inter-examiner reliability between the Author and the benchmark BASCD
examiner was measured.
For the fieldwork the recorder
was trained in recording data by the Author who conducted all
examinations. An assistant was responsible for co-ordinating the
children.
Subjects Study Population
All 12 yr olds in Montserrat
were invited to be part of the survey which was carried out on 14th
March 2006. In total there were 46 pupils who all attended the only
secondary school on the island. Positive consent was sought 2 days
prior to examination and 32 students responded positively. The
remaining students failed to return consent forms from parents and were
therefore not permitted by the school authority to take part. This was
in
accordance with exclusion criteria of the study.
Equipment
- CPITN probe Disposable
non-latex gloves
- Sterile cotton gauze Data
recording sheets
- Mouth mirror, Plane No.4 Desk
- Dental face shield
Standardized
light source
Examination procedure
Children presented to
examination room in no particular order. They were first asked to
complete the “Child Oral Health Questionnaire”. The
assistant recorded name, date and parental occupation on data forms.
Each child was given a data form and directed to the examination. Data
forms were handed to recorder who then went on to record data as
instructed by examiner.
Each child was asked to lie on
the desk in a supine position with examiner positioned directly behind.
A Tikka Petzl (3LED) head lamp was used for a light source. Examination
packs consisting of a sterile CPITN probe and sterile gauze and
disposable mirrors were unwrapped by dentist for each child.
Tooth surfaces were dried with
sterile cotton gauze and examined in a standard order as specified by
the study protocol. Following the examination all instruments were
placed in a “dirties” container and gloves disposed
of in a clinical waste bag. No radiographs were taken.
Any child requiring treatment
was identified and parent informed and advised by letter to seek
appointment at the local dental clinic.
Cross infection control
A standard cross infection
prevention protocol was followed. The examiner wore a face shield
through out the examination and gloves were changed after each patient.
Intra-examiner reliability
Five subjects were re-examined
and statistical test applied to determine intra-examiner reliability.
Data analysis
Data were processed using
Dental Survey Plus 2 version 2.1 and Statistical Package for Social
Sciences (SPSS version 14) software for the purpose of obtaining
descriptive statistics.
Results
Calibration of examiners
High levels of agreement were
recorded (Kappa = 0.81) between the BASCD ‘gold
standard’/benchmark examiner and the Author (Fergus CE). Five
child subjects were examined and scored using the DMFT Index and the
BASCD caries criteria.
Characteristics of the sample
Of the 46 twelve-year-olds in
Montserrat 32 participated in the survey. This gave a response rate of
69%. A description of the participants by gender and parental
occupation is given in Table 1. There were slightly more boys than
girls.
Table 1. Distribution
of
12-year-old participants by gender and father’s occupation
|
|
No. of children |
% |
| Gender |
Male |
18 |
56 |
|
|
|
|
|
Female |
14 |
44 |
|
|
|
|
| Father's occupation |
Legislators |
1 |
3 |
|
Professionals |
7 |
22 |
|
Technicians |
3 |
9 |
|
Clerks |
2 |
6 |
|
Service workers |
5 |
16 |
|
Skilled agricultural |
2 |
6 |
|
Craft & Trade |
6 |
19 |
|
Plant & Machine |
3 |
9 |
|
Elementary occupations |
0 |
0 |
|
Armed Forces |
0 |
0 |
|
Not given |
3 |
9 |
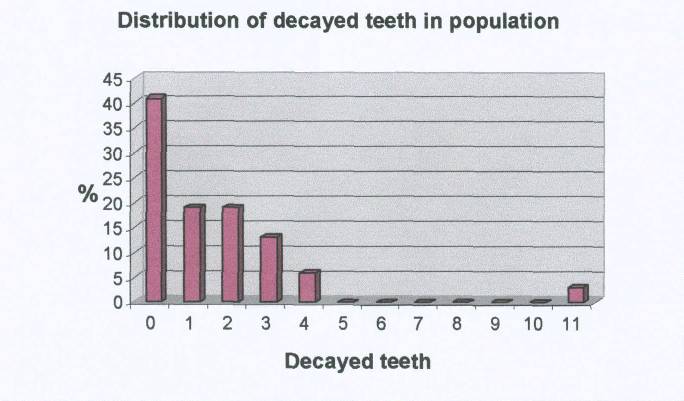
Caries experience
The sample of 12 year olds had
a mean DMFT of 1.91 (C.I. 1.05 to 2.76), (Table 2). Fifty-nine percent
had experience of decay in one or more teeth (DMF>0) (See Figure
1). Conversely only 41% of the children were caries free. One child
recorded with a DMFT of 11 (Table 3). All children with caries
experience were seen to have active, untreated caries (D>0) and
therefore normative treatment need. Few restorations were recorded
deriving a Care Index of 16%. Very few extractions had taken place. The
participants had an average of 25.69 (C.I. 24.8 to 26.58) sound teeth.
Table 2. Caries
experience of
12-year-olds in Montserrat
|
Mean |
Standard Deviation |
Confidence Interval |
| D |
1.53 |
2.16 |
0.75-2.31 |
| M |
0.06 |
0.25 |
-0.03-0.15 |
| F |
0.31 |
0.64 |
0.08-0.54 |
| DMFT |
1.91 |
2.37 |
1.05-2.76 |
|
|
|
|
| Care
Index % |
16 |
|
|
Figure 1:
Relative Distribution
of decayed teeth in 12-yr-old population
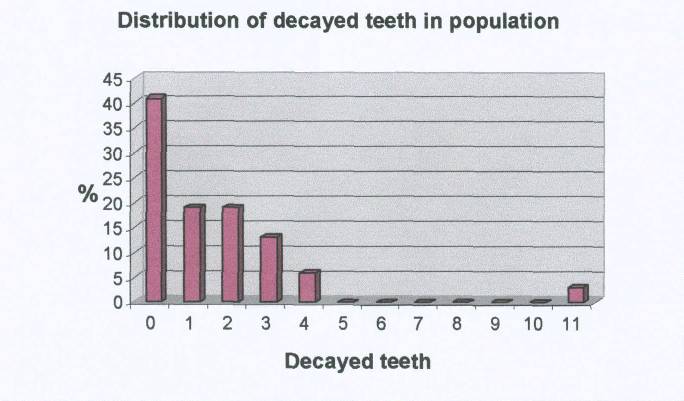
Table 3. Relative
Distribution of DMFT scores in 12-year-old population
| DMFT |
Number |
% |
Cum |
Cum % |
| 0 |
13 |
40.63 |
0 |
40.63 |
| 1 |
3 |
9.38 |
13 |
59.38 |
| 2 |
6 |
18.75 |
19 |
78.13 |
| 3 |
3 |
9.38 |
25 |
90.63 |
| 4 |
5 |
15.63 |
29 |
96.88 |
| 5 |
0 |
0.00 |
31 |
96.88 |
| 6 |
1 |
3.13 |
31 |
96.88 |
| 7 |
0 |
0.00 |
31 |
96.88 |
| 8 |
0 |
0.00 |
31 |
96.88 |
| 9 |
0 |
0.00 |
31 |
96.88 |
| 10 |
0 |
0.00 |
31 |
96.88 |
| 11 |
1 |
3.13 |
32 |
100.00 |
Caries experience and
socio-demographic characteristics
Tables 4 and 5 show the
breakdown of caries experience according to gender of the child, (Table
4) and the occupation of the father, (Table 5). In both cases numbers
of children in the survey are too small for significance testing.
However, there does not appear to be any difference in overall caries
experience between males and females, but there is a trend towards
greater caries experience in non-professional groups. Three children
did not give a paternal occupation (Table 1).
Table 4. Caries
experience of 12 year olds by gender in Montserrat [Mean (S.D.)]
| Gender |
D |
M |
F |
DMFT |
Confidence Interval |
Sound Teeth |
| M |
1.39 (2.64) |
0.06 (0.24) |
0.28 (0.67) |
1.72 (2.93) |
0.27-3.18 |
25.56 (3.07) |
| F |
1.71 (1.38) |
0.07 (0.27) |
0.36 (0.63) |
2.14 (1.46) |
1.30-2.99 |
25.86 (1.46) |
| Overall mean |
|
|
|
|
|
25.69 (2.47) |
Table 5. Caries
experience of 12 year olds by father’s occupation in
Montserrat [Mean (S.D.)]
| Parent occupation |
D |
M |
F |
DMFT |
Sound Teeth |
|
Legislators |
1 |
0 |
0 |
1 |
27 |
| Professionals
|
1.29 |
0.14 |
0.29 |
1.71 (2.43) |
25.57 |
| Technicians |
1 |
0 |
0 |
1 (1) |
24.33 |
| Clerks |
1 |
0 |
1 |
2 (2.83) |
26 |
| Service workers |
0.6 |
0 |
0.4 |
1 (1.41) |
27 |
| Skilled agricultural |
3 |
0 |
0 |
3 (1.41) |
25 |
| Craft & Trade |
3 |
0.17 |
0.17 |
3.33 (3.93) |
24.67 |
| Plant & Machine |
0 |
0 |
0 |
0 |
28 |
| Elementary occupations |
- |
- |
- |
- |
- |
| Armed Forces |
- |
- |
- |
- |
- |
| Not given |
2.33 |
0 |
1 |
3.33 (1.15) |
24.67 |
Quality of life data
Table 7 shows the distribution
of some responses to individual items on the Child Perceptions
Questionnaire for the 32 children surveyed. Most children (78%) rated
their oral health as “good” or better. The worst
commonly reported items were breathing through the mouth, slow eating,
food sticking between teeth, feeling upset or nervous about appearance
of teeth, difficulty doing homework because of problems with the mouth
or teeth and difficulty drinking or eating foods. A lower score
represents a lesser impact on QoL than a higher score.
Table 6. Descriptive
statistics
for the CPQ
| Jokovic
A; Locker D; Stephens M; Kenny D; Tompson B; Guyatt G (2002)
Validity and reliability of a questionnaire for measuring child
oral-health-related quality of life,
Journal of dental research
81(7): 459-63. |
|
Males
(19) |
Females
(13) |
Total |
Jokovic
et al. 2002 |
| QoL
|
Mean
|
SD
|
Mean
|
SD
|
Mean
|
SD
|
Mean
|
SD |
| Oral Symptoms
|
3.00
|
3.27
|
3.15
|
2.44
|
3.06
|
2.92
|
6.3
|
3.4
|
| Functional Limitations
|
7.61
|
6.04
|
9.82
|
6.98
|
8.45
|
6.39
|
6.7
|
4.9
|
| Emotional Well Being
|
6.89
|
4.97
|
6.23
|
5.23
|
6.63
|
5.00
|
6.4
|
5.7
|
| Social Well Being
|
7.00
|
6.10
|
5.92
|
7.38
|
6.56
|
6.55
|
6.9
|
6.4
|
| Total
|
24.28
|
18.01
|
23.44
|
22.15
|
24.00
|
19.06
|
26.3
|
16.7
|
Table 7. Results of the
CPQ: Scores for some items of health impact on QoL
| Item |
Excellent |
Very Good |
Good |
Fair |
Poor |
|
N (%) |
| Oral Health |
7 (21%) |
7 (21%) |
12 (36%) |
5 (15%) |
2 (6%) |
|
|
|
|
|
|
|
Not at all |
Very Little |
Some |
A lot |
Very much |
|
N (%) |
| Life overall |
18 (55%) |
10 (30%) |
2 (6%) |
1 (3%) |
2 (6%) |
|
|
|
|
|
|
|
Never |
Once/twice |
Sometimes |
Often |
Everyday/Almost every day |
|
N (%) |
| Upset |
11 (33) |
7 (21) |
8 (24) |
7 (21) |
| Food stuck between teeth |
5 (15%) |
11 (33%) |
11 (33%) |
3 (9%) |
3 (9%) |
| Difficulty doing homework |
18 (55) |
6 (18) |
3 (9) |
5 (15) |
1 (3) |
| Breathing through mouth |
9 (27) |
10 (30%) |
4 (12%) |
6 (18%) |
3 (9%) |
| Slow eating |
14 (42) |
5 (15%) |
8 (24%) |
1 (3%) |
5 (15%) |
Measurement of examiner
reliability
A randomly selected 5 of
the 32
subjects were re-examined at the completion of the main survey. Kappa
was used to determine intra-examiner reliability. The result of the
Kappa test was a score of 1, perfect agreement
Discussion
Caries Experience
The results of the study
indicate that the sample of 12 year olds examined have a mean DMFT of
1.91. This indicates that Montserrat has achieved the oral health goal
set by WHO of reaching a mean DMFT score of ≤3 by 2000
(Fédération Dentaire Internationale, 1981; WHO,
1988).
The mean number of Decayed
teeth being 1.53 (CI 0.75 to 2.31) contributes the highest proportion
of the total figure (D=1.53, M=0.06, F=0.31). The sample of 12-year-old
children had on average in excess of one an a half teeth with an
untreated cavity. The majority of children examined (59% with
D>0) were experiencing some form of active decay thus requiring
(professionally judged) treatment. Active caries (D component) was
measured at an advanced stage of the carious process when there was
clear visual dentinal involvement. This does not relate to treatment
need directly. There is recognised large underscoring in converting the
‘D’ component, in epidemiological studies, to
actual treatment need [3]. The indication is that there were quite high
levels of untreated decay amongst this population of children examined
and consequently high normative needs. This may imply that current
services are failing to meet this need.
The filled component of the
DMFT score was also fairly small at, 0.31 (0.64) and this was also
reflected by a low Care Index of 16%. The Care Index measures the
number of filled teeth in relation to dental disease and can therefore
gives an idea of the level of restorative care or treatment services
being provided. The Care Index is comparatively low when set against
the same age group in the UK. The 2000/01 BASCD study of 12 year olds
in England reported a Care Index was 48%. It can be argued that it is
inappropriate to compare a developing island state with a developed
country but this comparison gives an indication of the standard that
Montserrat should aim at. The other reality is that there is a lack of
regional data which goes beyond quoting DMFT to actually examining the
amount of care and describing treatment needs and amount of care being
delivered. Based on the information collected, that there was high
active caries and little restorative care in the children examined, it
is reasonable to presume that the free government service in Montserrat
may be being underutilized.
The mean number of Missing
(extracted due to caries) teeth was the lowest component, being less
than 1. This may reflect the following: 1) children are retaining their
teeth 2) children are not having extractions as a treatment for dental
decay which may be because much of the decay could be restored. 3)
children are not accessing dental care and receiving treatment.
Gender Distribution
It is difficult to
determine
from this small sample size whether the higher DMFT scores observed in
females was statistically significant. Nonetheless in the studies that
observe a higher caries experience among girls they tend to attribute
it to females having a greater propensity for sweet foods or poorer
dietary habits [4]. The explanation put forward by the author is only
speculative and may not be scientifically supported. No significant
differences in the dentinal caries experience of boys and girls were
reported in the Child Dental Health Surveys, UK, 2003 [5]. However
girls were more likely to brush twice a day than boys [6]. Such
findings have implications for how dental health interventions are
delivered.
Socioeconomic Status
The father’s
occupation was used as an indirect measure of child socioeconomic
status. Montserrat does not have distinct social class system so this
proxy measure was used. The occupation classification was based on the
International Standard Classification of Occupations (ISCO88) which
classifies jobs into occupational groups according to the similarity in
the skill level and the skill specialisation of the tasks and duties
performed. For convenience purposes the “Major”
ISCO grouping was used which is quite broad. It merges many occupations
together and doubtlessly conceals many important details.
The father’s
occupation was chosen because father is often regarded as the head of
household. However, there are many single parent families in Montserrat
where the mother is the sole provider. Omitting the mother’s
occupation may exclude relevant information and introduce bias [7]. In
this study the children of professional fathers had lower caries
prevalence than children of non-professional fathers (Table 5).
Socioeconomic status has been linked with oral health status and indeed
there is evidence that persons of lower socioeconomic status often have
worse health than persons of higher socioeconomic status [8].
This introduces the concept
of
a social gradient in health that has been expressed by many
researchers. It refers to the fact individuals at the top of the social
strata have better health than those immediately below them on the next
strata and this continues down the social scale or employment hierarchy
[9 Sheiham and Watt 2000].
These authors reported that
from 1978-1988 the mean number of decayed teeth in social classes IV
and V in the UK was 1.8 compared with 0.8 in the upper social classes.
This disparity in caries
experience between children from higher and lower socioeconomic
households although not quite marked should be monitored or explored
further. It is important that any gap be closed and that those at the
lower end are not disadvantaged by inequalities.
Quality of Life
The quality of life data
showed
most children regarded their oral health as “good”
or better. They also reported a low level of oral symptoms despite
having increased levels of functional limitations. This was interesting
to note. One explanation could be that the children did have
significant oral symptoms but had managed to cope with them. Blaxter
reported that 71% of persons with health problems described their
health as good or excellent in the National Health and Lifestyles
Survey [10 Blaxter 1990].
Social
determinants/Inequalities
Many researchers now focus
on
social determinants. It is thought that the broader determinants such
as economic and environmental factors have far reaching influence
ultimately affecting individual habits and behaviours. Good oral
hygiene habits and dietary practices will flourish in a supportive
environment, where such practices are the norm, where family and
community networks can shape habits and persons have access to
essential service and goods necessary for maintaining acceptable
standards of living and sustaining the good habits [11 Watt 2005].
Poor living conditions,
lack of
housing, unemployment, educational attainment are all causes of health
disparities. While it was not the aim of this study to explore the
reasons for the differences in oral health the following are points for
consideration:
- There has been severe
economic
downturn coupled with a rising cost of living following the volcanic
disaster.
- Many persons are still
facing
housing concerns having lost homes or having been forced to abandon
homes
- Small numbers of persons
are
living in volcanic housing developments which are in need of
restoration.
However, it can be argued
that
area deprivation is not a valid indicator as the entire population is
now dwelling or living in a more defined area of the country which can
be regarded as more homogenous. The essential action is to unearth the
“causes of the causes” [12 Sheiham and Watt 2003].
Oral health data from a
study
in New Zealand revealed significant association between higher caries
experience of an individual at age 26 and low paternal socioeconomic
position [13 Poulton et al. 2002]. This shows that adverse events in
childhood can have the impact later in life [14 Bartley et al. 1997].
Equally an argument can be made for positive interventions early in
life with the aim that later outcomes should be positive.
Significance of CPQ
The other concerns of the
children such as difficulty eating, being self conscious about
appearance should be considered. At face value they may not be regarded
as life threatening and could easily be dismissed by health planners
particularly when compared with conditions such as diabetes melitus and
cardiovascular disease. Quite a high percentage of children reported
feeling upset or nervous but these concerns are more personal in nature
and do not necessarily have a major impact on the society. Health
planners are challenged with convincing relevant authorities that these
valid concerns requiring attention. In fact they are all components of
the pubic health problem of dental caries. The challenge comes with
attempting to quantify, directly measure or assign a value or weight to
such concerns for the benefit of funding agencies or financial
departments who evaluate things in dollars and cents. Perhaps if these
concerns are quantified in terms of days lost from school, or in the
case of an adult days lost from work then the threat to economic
stability can be better assimilated or judged by those in authority.
While lowering the DMFT
will be
desirable and will provide a global indicator of the health status it
maybe of more value to the patients being served to be painfree, to be
able to eat without difficulty and to be able to work well in school.
These results can inform planning goals, objectives or more
specifically become outcome indicators.
Those children with higher
caries experience reported a greater impact on their QoL. This
difference was almost twice as much than those who were caries-free.
Although no significance testing was performed these results are
similar to the findings of other studies which highlight the impact of
oral disease on daily activities. Older adults in South Australia
reported greater levels of social impact on quality of life as a result
of being edentulous [15 Slade and Spencer 1994] .
Public Health Strategies
The success of salt
fluoridation in Jamaica [16] and proven effectiveness of water
fluoridation [17] lend support to adopting these options in Montserrat.
However, with a mean DMFT score of 1.91 at age 12, it may not be
justifiable to implement these programmes without further detailed cost
benefit analysis. It maybe equally worthwhile to evaluate current oral
health interventions, make modifications which are scientifically sound
before implementing these population based strategies. A combination of
oral health promotion activities (dental education, toothbrushing
campaigns) and restorative care for all, together with services
directed at those children at higher caries risk could be implemented.
A valid and feasible
strategy
for tackling this problem and convincing financial bodies whether
governmental or non-governmental is to implement the Common Risk Factor
Approach (CRFA) [9]. In this way several public health diseases are
simultaneously targeted by dealing with a few common risk factors. In
this instance diet is the risk factor for dental caries as well as for
diabetes mellitus, cardiovascular disease. Such a strategy involves
collaborative partnerships with other health and governmental
departments.
Study Limitations
A response rate of 69% was
achieved in this study. A better response rate would have been more
desirable given the small population size. However, study criteria
regarding consent had to be adhered to. Omitting the 14 children who
failed to return consent letters would likely result in omission of
important details and introduce bias. The small numbers also made it
difficult to perform any meaningful statistical analysis. Using
occupation as a measure of socioeconomic status could have been
limiting as it fails to acknowledge other dimensions (educational
level, income).
Conclusion
It is difficult to compare
Montserrat’s DMFT of 1.93 with that of regional islands as
the data was collected at different periods (Refer to Table 1). Many of
the islands have scores range from 0-6 suggesting that Montserrat is
not differing greatly or experiencing greater disparity than its
regional neighbours. It is important not to fall behind. Despite this
there is no place for complacency as high levels of untreated decay
exist amongst 12-year-olds in Montserrat. This indicates that there is
a need for restorative care from the professionals as well as an
existing need for care by the individual. This gap between the
professional need and patient need needs to be bridged. The barriers
preventing this must be identified. It could be something easily
identifiable such as fear, issues of accommodation or something more
complex as patient perception of illness and disease.
The low Care Index suggests
that the current service is falling short in their mission of providing
health to the community. Remuneration is via a salaried payment system
and one of the faults of such a system is under-treatment. This is just
one of many possible explanations being proffered.
Small numbers make it
difficult
to ascertain any differences between male and female oral health but
this can be monitored to ensure that no inequalities are created.
It is not apparent what
role,
if any, the social and environmental determinants within the community
are playing in disease causation. It is also not certain whether
economic downturns and housing issues are factors but further research
will have to be done on this.
Children are experiencing
significant disadvantage as a result of oral conditions or disease.
This should not be ignored or trivialised. Inequalities between
children of different socioeconomic status is evident from the study
but difficult to determine significance.
Recommendations
Montserrat should aim to
develop a comprehensive oral health policy as a matter of priority.
Special emphasis could be given to oral health of young persons.
Current oral health practices and policies need to be evaluated and
modified where necessary. The community, general health departments and
other stakeholders should be engaged in the policy development. The
benefit of conducting a health needs assessment should not be ignored
provided resources are available. The results of this study can serve
as a foundation for persuading health authorities to give oral health
greater priority and can guide general and local clinic policy
development or decisions. Additional surveys of children should be
performed for 5 and 15 year olds to get a more balanced representation
of the state of children’s health. A move towards more
evidenced-based dentistry is necessary. Broad areas for attention
include diet, dental education and toothbrushing programmes in
supportive environment. Urgent attention needs to be given to children
with active caries. This could be part of a targeted approach discussed
earlier. Adopting a CRFA toward health is highly recommended and this
necessitates collaborative partnerships with health departments. In the
long-term dental health providers should work with other governmental
departments to influence school nutrition policies, food importation
and production regulations and consumer education with respect to
healthy food choices. The government has a responsibility to ensure and
maintain acceptable living standards by reducing social, economic and
environmental and inequalities. Health is political.
References
1. Pine CM,
Pitts NB,
Nugent
ZJ. British association for the study of community dentistry (BASCD)
guidance on the statistical aspects of training and calibration of
examiners for surveys of child dental health. A BASCD coordinated
dental epidemiology programme quality standard. Community
Dental Health
1997; 13 (Suppl 1): 18-29.
2. Pine C,
Burnside G.
BASCD
Trainers’ Pack for caries prevalence studies.
University of
Dundee, Dundee 2004.
3. Nuttall N
M. Capability
of
national epidemiological survey to predict General Dental Service
treatment. Community
Dentistry and Oral Epidemiology
1983; 11: 296-301.
4.
Okeigbemen SA. The
prevalence of dental caries among 12 to 13-year-old school children in
Nigeria: report of a local survey and campaign. Oral
Health and
Preventive Dentistry 2004; 2:
27-31.
5. Pitts NB,
Chestnutt IB,
Evans D, White D, Chadwick B, Steele JG. The dentinal caries experience
of children in the United Kingdom, 2003. British
Dental Journal 2006;
200: 313-320.
6. White DA,
Chadwick BL,
Nuttall NM, Chestnutt IG, Steele JG. Oral health habits amongst
children in the United Kingdom in 2003. British
Dental Journal 2006;
200: 487-491.
7. Zurriaga
O,
Martinez-Beneito
MA, Abellan JJ, Carda C. Assessing the social class of children from
parental information to study possible social inequalities in health
outcomes. Annals of
Epidemiology 2004; 14: 378-384.
8. Watt R,
Sheiham A.
Inequalities in oral health: a review of the evidence and
recommendations for action. British
Dental Journal 1999; 187(1):
6-12.
9. Sheiham
A, Watt RG. The
common risk factor approach: a rational basis for promoting oral
health. Community Dentistry
and Oral Epidemiology 2000; 28:
399-406.
10. Blaxter
M. Health and
Lifestyles 1990; London:
Routeledge.
11. Watt RG.
Strategies and
approaches in oral disease prevention and health promotion. Bulletin
of
the World Health Organization
2005; 83(9): 711-718.
12. Sheiham
A, Watt RG.
Oral
health promotion and policy, in Murray JJ, Nun JH, Steele JG (ed.)
Prevention of Oral Disease
2003; 4th ed. Oxford: Oxford University
Press, pp. 245.
13. Poulton
R, Caspi A,
Milne
B, Thomson W, Taylor A, Sears M, Moffitt T. Association between
children’s experience of socioeconomic disadvantage and adult
health: a lifecourse study. The
Lancet 2003; 360(9346):
1640-1645.
14. Bartley
M, Blane D,
Montgomery S. Socioeconomic determinants of health Health and the life
course: why safety nets matter. British
Medical Journal 1997;
314: 1194-1196.
15. Slade
GD, Spencer AJ.
Development and evaluation of the oral health impact profile. Community
Dental Health 1994; 11: 3-11.
16.
Estupiñán-Day S, Baez R, Horowitz H, Warpeha R,
Sutherland B, Thamer M. Salt fluoridation and caries in Jamaica.
Community Dentistry and Oral
Epidemiology 2001; 29(4):
247-252.
17. McDonagh
MS, Whiting
PF,
Wilson PM, Sutton AJ, Chestnut I, Cooper J, Misso K, Bradley M,
Treasure E, Kleijnen J. Systematic review of water fluoridation.
British Medical Journal
2000; 32: 855-859.
Acknowledgements
I am indebted to the
students
who participated and their parents who consented.
The support and assistance
of
the principal and staff of the Montserrat Secondary School and the
Ministry of Education Health and Community Services were beyond
expectation.
Special thanks to the staff
of
the St. John’s Dental Clinic who assisted ably and
efficiently with examinations.
Thanks to Supervisors Dr
Nick
Kendall, Prof. Tim Newton and Dr. Blanaid Daly whose combined input was
invaluable and greatly appreciated.
©
Coretta
E. Fergus
HTML
last
revised 18th June, 2009.
Return
to
Conference
papers.